Author: Robert Gramling
Posted: June 2020
Mindfulness is “awareness that arises through paying attention, on purpose, in the present moment, non-judgmentally.”1
Efforts to promote mindfulness in healthcare result in physicians feeling more curious about their patients’ experience.2 When seriously ill patients feel this non-judgmental curiosity from their clinicians, they are likely to more fully engage in conversation and, ultimately, share more about what matters most to them in their medical context. Very little, however, is empirically known about the relation between clinician mindfulness and actual features of healthcare conversations with seriously ill people. Here, we evaluate the degree to which clinician self-ratings of mindfulness (i.e., Trait Mindfulness) is associated with key conversational dynamics of engagement.
We observed and audio-recorded the initial palliative care visit involving 231 patients with advanced cancer 54 palliative care clinicians in the Palliative Care Communication Research Initiative (PCCRI) cohort study. Each clinician participant completed the 5-item “attention” subscale of the Mindfulness Awareness and Attention Scale (MAAS)3 once at study outset. We used natural language processing of verbatim transcripts to identify the total number of conversational words and speaking turns. We defined a speaking turn as any stretch of uninterrupted speech. An “interruption” is any act that claims the speaking floor sufficiently for the transcriptionist to recognize. We used audio files to identify duration of the conversation.
If the clinical interaction was temporarily suspended, as might happen for a patient who needed help with bathing or a change of bedding, then that period of time was excluded from conversation duration. We calculated turn-taking rate as the number of turns divided by total minutes in conversation. We calculated average turn length as the number of total turns divided by the number of total words in the conversation.
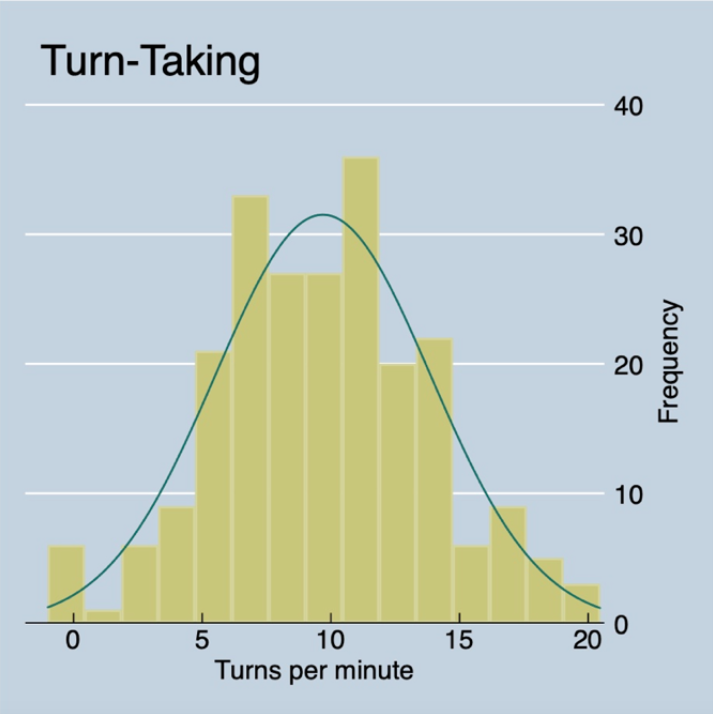
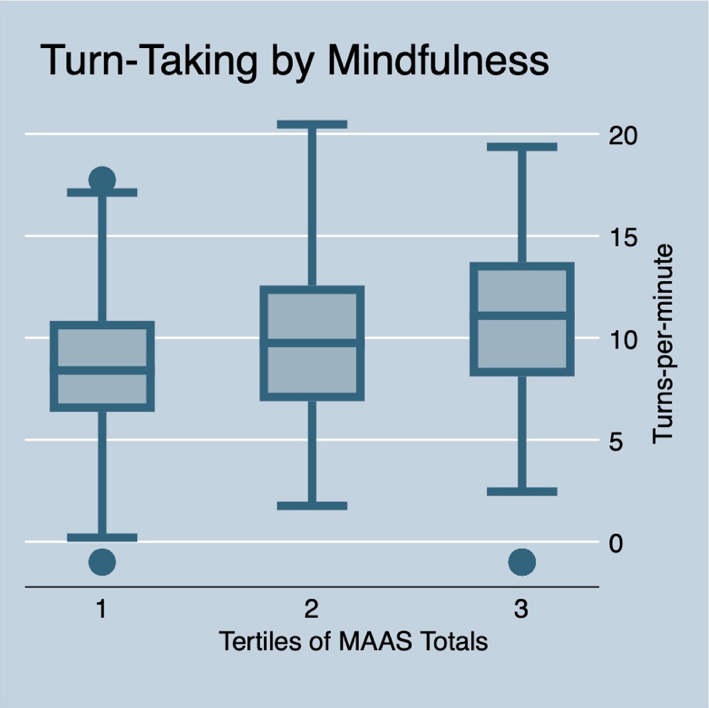
Possible MAAS scores range from 5 to 30; palliative care clinician MAAS scores spanned from 12 to 27 without an appearance of normality or clear inflection points. Therefore, we trichotomized MAAS summary scores into “Low” (<19), “Middle” (20 to 22) and “High” (>23). As shown in the figure to the right, rates of turn-taking demonstrated a near normal distribution. Higher levels of trait mindfulness demonstrated a dose-dependent relationship with higher turn taking rates (Figure below, ANOVA p-value=0.03). This pattern persisted across strata of clinician gender, patient gender and clinician years in practice. We did not observe an association between mindfulness and total number of words spoken during the conversation.
These findings suggest a relationship between clinician Trait Mindfulness and dynamics of conversational engagement with seriously ill patients. This analysis does not lend sufficient insight into to whether clinician’s self-rated Mindfulness reflects their actual internal state of Mindfulness nor whether increased rate of turn-taking affects the overall quality of these communication. Furthermore, our data are insufficient to fully address potential confounding by other clinician characteristics that might impact communication actions (e.g., conversational self-efficacies). Nonetheless, these findings lend support for the conceptual value of mindfulness in serious illness communication and highlight the need for further scientific attention.
References
1. Jon Kabat-Zinn. www.mindful.org
2. Scheepers RA, Emke H, Epstein RM, Lombarts KMJMH. The impact of mindfulness-based interventions on doctors’ well-being and performance: A systematic review. Medical Education. 2020;54(2):138-149.
3. Park T, Reilly-Spong M, Gross CR. Mindfulness: a systematic review of instruments to measure an emergent patient-reported outcome (PRO). Quality of Life Research. 2013;22(10):2639-2659.