Author: Robert Gramling
Posted: August 2019
Time to Talk?
As our science of palliative medicine grows, it is safe to put our empirical nickel down on two things. First, specialty palliative medicine consultation improves the experience, quality-of-care and quality-of-life among seriously ill persons* and their families (Kavalieratos et al., JAMA, 2016). Second, current and projected demand for specialty palliative medicine far exceeds capacity (Kamal et al., American Journal of Medicine, 2017). This set of circumstances presents a compelling challenge for us to scale up the active ingredients of specialty consultation to meet our public health need. Many indirect and some direct observation findings point to high quality conversations as a pivotal component of our value. Little, however, is actually known about the content and processes of these human interactions that confer value nor how the environmental, inter-personal and intra-personal contexts influence their effectiveness.
As a person who cherishes having these types of conversations, studying them and advocating for interventions to promote them in routine clinical practice, I often contemplate the role of talk time. As we move to a system of healthcare financing that pays for “value”, how will we value time for us to talk with one another? This brief analysis is a nod toward cultivating a scientific base from which to address this crucial policy question.
We don’t yet understand the specific features of conversations that confer “value”, how exactly to measure them, nor whether talk time affects them. However, two conceptual domains stand out as reasonable places to start. The first is creating space to hear the seriously ill person’s voice. (Tulsky et al., JAMA Internal Medicine, 2017; Gramling et al., Journal of Pain and Symptom Management. 2016) The second is offering the opportunity to talk about clinical expectations for prognosis in order to provide sufficient context to align personal values with available treatments. (Norton et al., Research in Nursing and Health.2013; Gramling et al., Journal of Palliative Medicine. 2019)
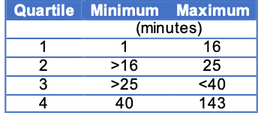
Here, we use data from the Palliative Care Communication Research Initiative. This analysis comprises 231 audio-recorded initial palliative care consult conversations between unique hospitalized patients with metastatic cancer and 54 specialty palliative care clinicians. The cumulative talk time is approximately 14,000 minutes with quartiles of direction shown in the table to the right. Using these data, we measure three things.
First, we record the number of minutes from beginning to end of the observed conversation audio file. Second, we use Natural Language Processing of verbatim transcripts to count the number of times the patient (or proxy, if the patient is not present) speaks. Anytime that a person is interrupted, this changes a speaker turn. Third, we trained human coders to reliably identify the number of times that a speaker turn includes a prognostic expression – defined as any “prediction about a future health state or event.” (Ingersoll et al., Patient Education and Counseling. 2019)
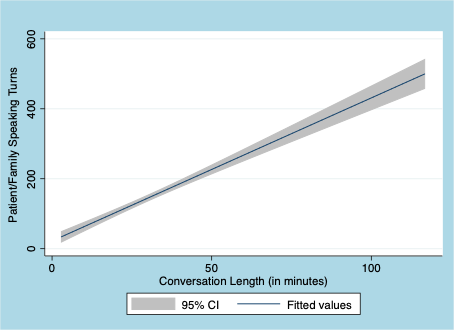
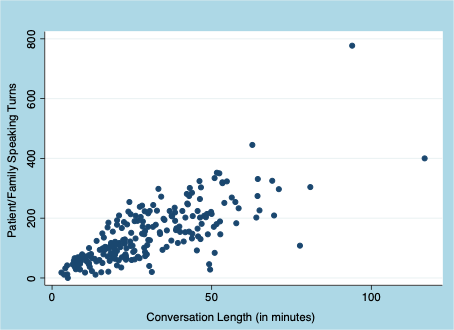
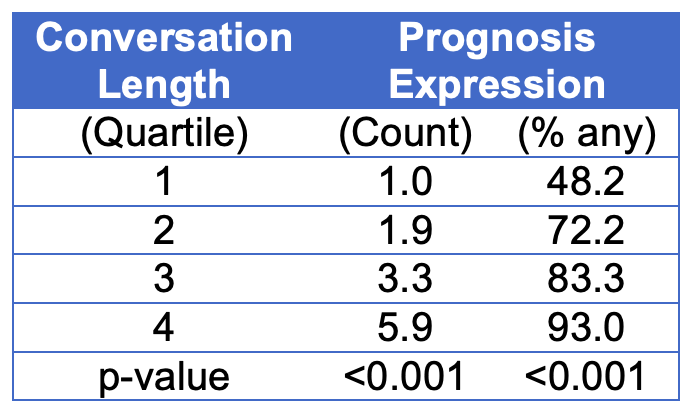
As shown in the scatterplot (Figure One) and fitted linear model (Figure Two), we observed a strong direct association between the time in conversation and the number of patient/family speaking turns. On the one hand, these findings are not surprising. A logical person would assume that the more time people have in conversation, the more each speaks. However, other direct observation studies have not found this strength of correlation because physicians tend to hold the speaking floor far longer than patients. (Chhabra et al., Patient Education and Counseling. 2013) Under such conditions, the rate of patient speaking turns would demonstrate a less impressive slope in relation with overall conversation time than we observe here. We also observed a strong dose-response relationship between talk time and sharing of prognosis information. (see Table Two)
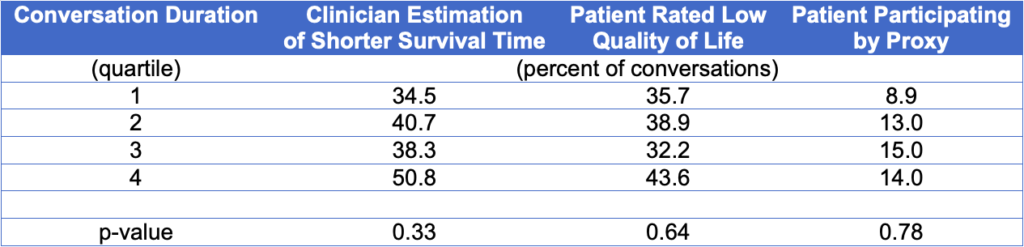
Observational associations are prone to “confounding by indication”, meaning that the clinical reason for an action to have happened (e.g., prescribing a medication, doing a test) might not be readily controlled for with the data available to the analyst. In these associations shown above, it is possible that the controlling for the reasons behind participants having a longer conversation might change the observed association with rates of patient speaking or prognosis sharing. In these preliminary findings, we explored potential confounding by the clinician’s judgment about the proximity of death, the patient’s rating of their overall quality of life, and whether the conversation was happening by proxy (meaning that the patient was not participating directly). Interestingly, none of these factors appeared to be associated with talk time (see Table Three) and, subsequently, did not confound these two associations. In forthcoming work, we will develop more robust propensity matching methods to address confounding of association between talk time and conversation features.
These collective observations are a preliminary glimpse into the relationship between talk time and conversation quality. These findings do not lend themselves to inferences about causality. In fact, if we were to conclude that systematically exposing people to longer serious illness conversations would be “good”, then that would likely cause unintended harm. Sometimes an effective “arc” of a palliative care serious illness conversation happens within minutes. Other times, it evolves over many visits spanning days, weeks, or months. Indeed, good communicators need to cultivate and maintain a keen sense of situational awareness to evaluate and re-evaluate the healing or toxicity of any conversation. However, what these findings suggest is that having the opportunity to remain in conversation for longer periods of time than typically afforded in modern healthcare is of empirical value, deserves more research and is crucial to effective scaling of palliative care.
*Kelley et al., Journal of Palliative Medicine. 2018 definition: ‘‘Serious illness” is a health condition that carries a high risk of mortality AND either negatively impacts a person’s daily function or quality of life, OR excessively strains their caregivers.